Key Concepts
- Health System
- Health Systems Strengthening
- Primary Care
- Secondary Care
- Tertiary Care
- Governance
- Service Delivery
- Responsiveness
- Access
- Quality
- Safety
- Coverage
- Efficiency
- Financial Risk Protection
- Public
- Private, For Profit
- Private, Not For Profit
- NGO
Prelim Engagement
- Watch this short video: https://youtu.be/uB2EzlKcRIA
- Listen to this short podcast: https://www.thelancet.com/pb-assets/Lancet/stories/audio/lancet/2018/TL_Sep_18_health_systems-1536155267440.mp3
- Watch this short video: On GPS: The UN Secretary-General on Covid (cnn.com)
Introduction
In this Section we will explore the concept of a health system. We will define the term Health System, examine its functions and organization and take a more indepth look at some examples of different types of health systems to look for similarities and differences. We will also take a look at the Public Health aspects of Health Systems and why and how we must Work Together to improve health. We return to one of the most important questions we must ask ourselves in Global Health, Why treat people…then send them back to the conditions that made them sick?
Figure 1:

In this section we will focus on the first part of this question, namely, Why treat people? What is involved in treating people? To answer that part of the question, we must understand the mechanism for treating people and that mechanism is the Health System.
A Brief History of Global Health Systems
The concept of a Health System is a relatively new idea in historical terms. Much of the history of Health Systems is tied to the history of medicine which first began in ancient Mesopotamia and Egypt (Porter, 1996). Hospitals were the first examples of Health Systems. Archaeological evidence indicates that the Romans first built hospitals within their forts to treat slaves and soldiers ( Merton, 2018). In addition both Christian and Islamic religions built hospitals in the major cities of their respective worlds. In both cases, they were created to care for sick people who did not have family or servants to take care of them. In the Middle Ages, the Plague or Black Death in Europe caused ‘growing state involvement in protection of health through measures such as imposing quarantines and isolating the sick. (Merton, p. 1867).
As the WHO notes: “Throughout the world, traditional practices based on herbal cures, often integrated with spiritual counselling, and providing both preventive and curative care, have existed for thousands of years, and often coexist today with modern medicine. Many of them are still the treatment of choice for some health conditions, or are resorted to because modern alternatives are not understood or trusted, or fail, or are too expensive. Traditional Chinese medicine can be traced back more than 3000 years, and still plays a huge role in the Chinese health system, as do its equally ancient equivalents in the Indian sub-continent and similar systems of belief and practice among indigenous African and American peoples.” (p.
Although hospitals have a much longer history than complete systems in many countries, few people living 100 years ago would ever visit one – and that remains true for many millions of the poor today. Until well into the 19th century they were for the most part run by charitable organizations, and often were little more than refuges for the orphaned, the crippled, the destitute or the insane. Even in industrialized countries, organized health systems in the modern sense, intended to benefit the population at large, barely existed a century ago. Lets turn to modern day understandings of Health Systems.
Health System Definitions
Let’s start with some very basic definitions. A system can be defined as a set of principles or procedures according to which something is done; an organized scheme or method. In Global Health we often use a systems thinking approach to understanding complex issues such as a Health System. Systems Thinking can be defined as the process of understanding who those things which may be regarded as systems influence one another within a complete entity or larger system as illustrated in Figure 2 below.
Figure 2
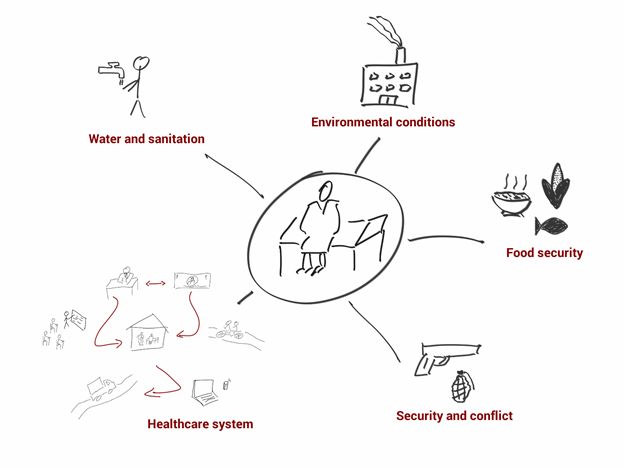
Here we see that the Health System is a part of or a subsystem of the larger context in which a person lives often referred to as the social and structural determinants of health described earlier in Section 1.4 of this Textbook.
A simple definition of a Health System is that it is the structure through which health services are delivered to individuals and populations. It is also the mechanism through which diseases, illnesses, conditions and injuries are managed in individuals and populations. It is important to note that a Health System is based upon a set of components that are inter-related as we will see throughout this Section. Health Systems are made up of people and organizations. This complexity can cause the system to be less efficient or effective. Here are a few formal definitions:
- The sum total of all the organizations, institutions and resources whose primary purpose is to improve health (WHO, n.d.)
- The combination of resources, organization and management that culminate in the delivery of health services to the population (Romer, 1991)
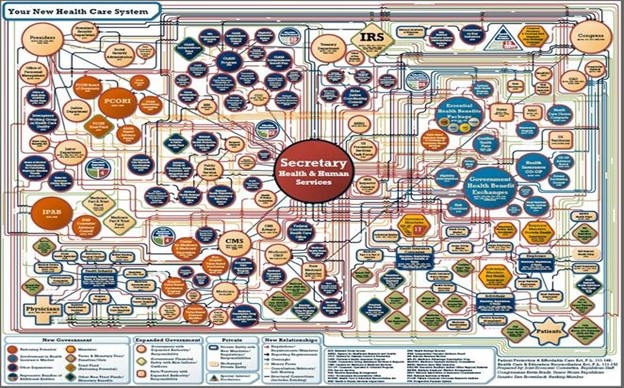
It is important to remember that systems, including Health Systems can be depicted as being very simple (Figure 3) to very complex (Figure 4)
Figure 3: A Simple Health System
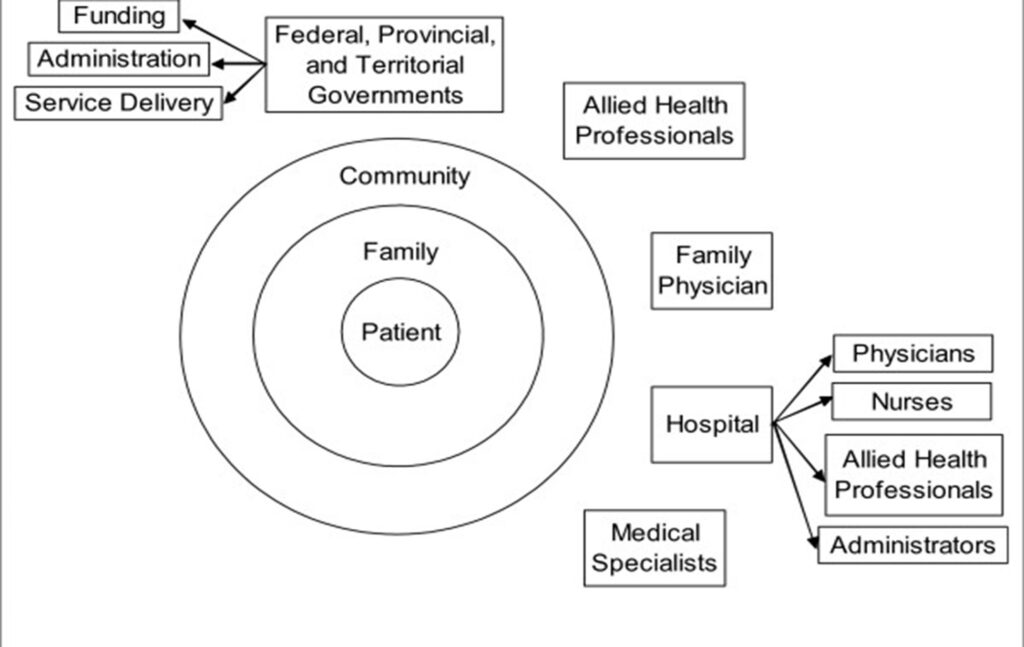
Figure 4: A Complex Health System
Goals of Health Systems
In the year 2000, the World Health Organization authored a World Health Report (WHR) entitled Health Systems: Improving Performance [Prelims i-ixx/E (who.int) ](WHO, 2000 ) This Report with the fifth in an ongoing of series of annually released WHRs that focus on a global health topic and includes an assessment of each country’s status on the topic. The 2000 Report lists the following goals for health systems:
- Good health
- Fairness of financial contribution
- Responsiveness to the population’s expectations
Importance of Health Systems
It is useful to have a foundational understanding of Health Systems in the study of Global Health because of the individual, demographic and economic trends that impact on how well country’s Health System is able to deliver its health care services to its population.
At the individual level, the health status of an individual is directly related to their ability to access to health care services provided by a Health System. Health Systems are the vehicle through which people have access to health services. If one does not have health care services available to meet their needs, their health status will decline and this will have significant implications for their individual and family’s ability to be hold a job, go to school or remain out of poverty. As we saw in Section 1.7 on Ethics and Human Rights earlier in this Textbook, people should have a human ‘right’ to good health. Access to health services helps to increase health status. As health status rises in a population, so does the economic productivity of a country as we learned earlier in Section 1.4 regarding the principle of the health-development linkage we see in global health. From a demographic perspective recall that we explored the Demographic Transition in Section 1.3 and learned that the world’s population is increasing aging. This transition has implications for Health Systems as they must be flexible to meet the health care service needs that accompany the increased rates of Non-Communicable Diseases that are most prevalent in older populations (a consequence of the Epidemiologic Transition). From an economic perspective, individual households spend a significant amount of their budgets on health care services. Similarly, countries spend large shares of their Gross National Income on their Health System. In summary, a major goal of the Health System in all countries is to attain the best possible health status for its population in a fair and equitable manner at the lowest cost possible.
Organization of Health Systems
Health Systems can be categorized according to the levels of service they provide. Each of these levels involves a set of agencies and organizations that develop, finance and regulate health care services delivery. The three levels of care are primary, secondary and tertiary. While these levels are present in most Health Systems, the economic status or income of a country determines what kinds of services are provided.
Levels of Care
| Levels of Care | Staffing & Services in Low Income Countries | Staffing & Services in High Income Countries |
| Primary Care | Medical Assistants, Nurses, Midwives; Family Planning, Maternal-Child Health, Diagnosis/Treatment of simple childhood & adult diseases & injuries, TB & Malaria | Physician is first point of contact and source of referral (gate-keeper); Prevention services, Diagnosis/Treatment of common diseases & injuries |
| Secondary Care | Physicians; above services and emergency obstetric care, Diagnosis/Treatment of general childhood and adult diseases. Basic emergency treatment and surgery | Physicians and General Hospitals; Basic emergency treatment and surgery |
| Tertiary Care | Physicians, Surgeons; above services and Treatment of complicated childhood & adult diseases, advanced emergency care, specialist surgery | Specialists in Specialized Hospitals; Specialty treatments such as oncology in cancer hospitals |
A note about the term Primary Care compared to Primary Health Care. In Section 1.7 we explored the concept of Primary Health Care which refers to an outcome of the Declaration of Alma Ata in 1978. The Declaration focused attention on health care as a human right and to the right of people to participate in the planning and implementation of health care. The concept of ‘health for all’ by the year 2000 has yet to be achieved but the notion that health care should be directed by the community remains a core principle in global health. Primary care, as noted above is the first level of health services.
Much debate has centered on whether one way of organizing a health system is better than another, but what matters about a system’s overall structure is how well it facilitates the performance of its key functions.
Functions of Health Systems
Based on the Goals of Health Systems described in the WHR 2000 report, Health Systems should have the following four functions:
- Provide health services for people to easily access (prevention, diagnosis, treatment and rehabilitation services)
- Generate resources (raise enough money) to be spent on health
- Pay for health services (financing) including providing insurance to protect against financial loss for individuals and families who are sick and need services
- Regulate and manage the health system (stewardship) through oversight functions known as governance
These functions can be achieved through a set of six building blocks, referred to as the Health System Building Blocks (see Figure 1 below)
Figure 3: Health System Building Blocks

Source: http://www.wpro.who.int/health_services/health_systems_framework/en/
The Health System Building Blocks taken together form a Framework for understanding the different parts of a Health System. You might look at the Framework as consisting of Inputs or Structures (left hand side), Throughputs or Processes (middle) and Outputs or Outcomes (right hand side). Lets look at each in a bit more depth to understand how they work together
Inputs/Structures
- Service Delivery: Good service delivery involves delivering effective and safe services to people when and where they need them with efficiency.
- Health Workforce: A well performing workforce consists of having a sufficient number of staff with appropriate training and the right mix of fields who are responsive, fair and efficient in the delivery of services given the available resources and circumstances.
- Health Information Systems: A well-functioning information system is one that delivers reliable and timely information on health systems performance including health determinants and health status.
- Medical Products and Technologies: Equitable access to essential medical products, vaccines and technologies that are of high quality, safe, effective and can be used at the lowest cost.
- Financing: Adequate funds that are raised for health that ensure people can access the services they need and are protected from financial impoverishment due to cost.
- Leadership/Governance: Involves ensuring that management, oversight and regulations are in place in an open and participatory manner that attends to accountability for maximizing health for the amount of money spent.
Throughput/Process
- Access: Provide persons with the ability to receive health care services by ensuring that people know where/what types of health care services are available to them
- Coverage: Try to cover all or as many persons as possible in the health system by ensuring that all people have some form of basic health insurance
- Quality: Ensure that health care services provided to people are of the highest quality (best standard of practice). For example, medications provided are not expired
- Safety: Ensure that health care services provided are safe for both patients and the health care workforce. For example, using procedures that minimize the possibility of infection
Output/Outcome
- Improved Health: Individual and population health status levels improve by using the health system and that there is equity in services provided among different groups. Advocate for the Right to Health
- Responsiveness: The needs of the individuals being served are considered in the services being offered
- Social & Financial Risk Protection: The costs of services being provided does not cause people to be denied services or become impoverished because of an inability to pay
- Improved Efficiency: Changes in procedures and policies in the health system to save money and to get as much health benefit for the amount of money spent
It is thought that if countries combine these blocks of the WHO Framework together, the result will be a Health System that improves health in equitable ways and achieves the goals for a Health System.
A note on Vital Registration: Recall that in Section 1.2 we were introduced to the concept of vital registration. Vital registration systems record births, deaths, and causes of death. An accurate system is key to having quality data on a population. Many low- and middle-income countries lack a vital registration system. Often there are cultural barriers to timely vital registration (i.e., not registering a birth until months after baby is born due to fears the baby may not survive).
Roles of Sectors in Health Systems
Here we begin by asking, “What are the roles and responsibilities of the public, private and non-governmental organizations (NGOs) sectors in Health Systems”?
| Role Type | Responsibilities in Health System |
| Public Sector (National, District, Province, State, Municipal) | Stewardship of the systemRaising the funds for the health systemMaking decisions about allocating those fundsEstablishing approaches to health insurance |
| Private, For-Profit Sector (District, Province, State, Municipal) | Involved in the provision of services including nonlicensed “medical practitioners” Involved in the operation of health clinics, hospitals, services, and laboratoriesCan partner with the public sector or work under contract to the public sectorIs involved in essentially all countries |
| Non Governmental Organization (NGO) Private, Not- For-Profit Sector (International, National, District, Province, State, Municipal) | Often involved in community-based efforts to promote better health through education, improved water and sanitationOften carry out health servicesCan partner with the public sector or work under contract to the public sector |
Provision of Health System Services
Which actors are involved? These include the health care workforce which provide the following health care services for diseases, illnesses, conditions and injuries.
- Preventive health services
- Clinical treatment services
- Rehabilitation services
- Pharmaceutical services
- Medical device production
- Health professions education
In studying Health Systems, it is useful to ask questions about the appropriate roles that each of these sectors represent and how the services provided are paid for. For example, is it more cost effective for the public sector to contract out the provision of primary care services to the NGO sector? Who should deliver these services? These types of questions and the consequences of the arrangements are part of understanding how the Health System is organized.