Key Concepts
- World Bank and World Health Organization (WHO) regions
- Income Groups (World Bank)
- Global Burden of Disease Rankings
- Disability
- Impairment
- HALE
- DALY
- YLL
- Demographic transition
- Epidemiologic transition
- Levels of Prevention
- Millennium development goals (MDGs)
- Sustainable development goals (SDGs)
Prelim Engagement
- Watch this short video clip on disease change over time:
Section 1.3.1 Understanding Key Global Institutions in the Field of Global Health
Throughout the course we will often reference the International Monetary Fund and the World Bank as leading and highly influential institutions driving global economic, social and health development policy and financing especially in countries without a lot of economic resources. What are these institutions with so much influence and what exactly do they do?
Watch the short video clip below to find out.
As the above video states, the World Bank is especially involved in the economic, social and health development of countries without a lot of economic resources. The World Bank also provides a tremendous amount of economic and health data on different economic and health outcomes in these countries.
You will recall in Section 1.2 in our discussion of descriptive epidemiology, that we concern ourselves with identifying Place, Person and Time. In the field of global health when we talk about Place, we are referring to different countries. We often use World Bank classifications to talk about different groups of countries, especially when we are comparing economic and health outcomes between different groups of countries.
World Bank
The World Bank classifies countries in two main ways:
- Geographic region
- Income group
There are seven World Bank geographic regions:
- East Asia and Pacific
- Europe and Central Asia
- Latin America and the Caribbean
- Middle East and North Africa
- North America
- South Asia
- Sub-Saharan Africa
World Bank Regions Map

If you are interested in learning about the specific countries in each World Bank region here is a link to an Interactive map:
https://dataviz.worldbank.org/t/DECDG/views/Worldbyregion2019/Worldbyregion?iframeSizedToWindow=true&:embed=y&:display_spinner=no&:showAppBanner=false&:embed_code_version=3&:loadOrderID=1&:display_count=n&:showVizHome=n&:origin=viz_share_linkWorld Health Organization
In addition to the World Bank’s Regions Map, the World Health Organization (WHO) also has its own classification of world regions.

There are four World Bank income group classifications. Countries are grouped into these classifications based on their gross national income (GNI) per capita. Examples of countries within each of the income group classifications is provided in Table 3.1 below. GNI per capita is a way to look at the country’s income divided by its population per year, and it is the clearest way to compare income per person in a country (OECD, 2021). World Bank Country Income Groups are as follows:
- Low-income countries: ($1,036 or less)
- Lower middle-income countries: ($1,036 and $4,045)
- Upper middle-income countries: ($4,046 and $12,535)
- High-income countries: ($12,536 or above)
Table 1.3.1 Representation of High, Middle and Low-income Countries
| World Bank Country and Lending Groups, 2021, Selected Countries | |||
| Low income ($1,035 or less) | Lower middle income ($1,036 and $4,045) | Upper middle income ($4,046 and $12,535) | High income ($12,536 or above) |
| Afghanistan | Côte d’Ivoire | Botswana | Aruba |
| Congo, Dem. Rep. | El Salvador | Brazil | Denmark |
| Haiti | India | Fiji | Israel |
| Korea, Dem. People’s Rep. | Moldova | Lebanon | Korea, Rep. |
| Syrian Arab Republic | Nepal | Mexico | Mauritius |
| Tajikistan | Tunisia | Russian Federation | Qatar |
| Yemen, Rep. | Ukraine | Turkmenistan | Singapore |
Section 1.3.2 Risk for Mortality
In Sections 1.1 and 1.2 we identified and defined the major global health concepts of disease, injury and conditions as well as rates for the key health indicators of life expectancy, mortality and morbidity. Here we will use graphics to illustrate how the concepts of person, place and time can assist in identifying risk among different group, detect groups at high risk and develop hypotheses about causes – that is to identify why groups might be at increased risk. As you look through these graphs, ask yourself who, when and where is there risk? Why?
Life expectancy at birth by World Bank income group

Rights: CC-BY
Risk Issues: People who have low income may have shorter life expectancy compared to other groups. Why?
Life expectancy at birth by World Bank Region

Rights: CC-BY
Risk Issues: People who live in Sub-Saharan Africa and South Asia may have shorter life expectancy compared to other groups. Why?
Maternal Mortality Ratio by World Bank Country Income Group

Risk Issues: Women who are pregnant or give birth who live in low income countries may have higher mortality rates compared to other groups. Why?
Maternal Mortality Ration by World Bank Region

Risk Issues: Women who are pregnant or give birth who live in Sub-Saharan Africa and South Asia may have higher mortality rates compared to other groups. Why?
Now its time for you to explore what happens with some of our other Mortality Indicators
Neonatal Mortality Rate by World Bank Income Group
Risk Issues: Infants of age of 28 days or less who live in low income countries may have higher mortality rates compared to other groups. Why?
Neonatal Mortality Rate by World Bank Region
Risk Issues: Infants of age of 28 days or less who live in Sub-Saharan Africa and South Asia may have higher mortality rates compared to other groups. Why?
Infant Mortality Rate by World Bank Income Group
Risk Issues: Children under 1 year of age who live in low income countries may have higher mortality rates compared to other groups. Why?
Infant Mortality Rate by World Bank Region
Risk Issues: Children under 1 year of age who live in Sub-Saharan Africa and South Asia may have higher mortality rates compared to other groups. Why?
Under-5 Mortality Rate by World Bank Income Group
Risk Issues: Children under 5 years of age who live in low income countries may have higher mortality rates compared to other groups. Why?
Under-5 Mortality Rate by World Bank Region
Risk Issues: Children under 5 years of age who live in Sub-Saharan Africa and South Asia may have higher mortality rates compared to other groups. Why?
Do you notice any patterns arising with regard to the mortality rates and regions for example?
Comparing Under-5, Infant and Neonatal Mortality Rates by World Bank Region

In this graphic, we see that the under 5 mortality rate is consistently the highest mortality rate followed by the infant mortality rate and the neonatal mortality rate. In addition, Sub-Saharan Africa and South Asia have the highest mortality rates when compared to the other regional groups. Again, we should ask always ask Why?
If you are interested in exploring how these key indicators change over time or with other population characteristics, here is an online tool: https://data.worldbank.org/
Section 1.3.3 Measurement of Disease Burden
Thus far we have measured disease burden from a mortality focus. In global health, we would also like to account for morbidity and how that may impact on mortality. In addition, we introduce another concept related to morbidity referred to as disability. A disability can be defined as a temporary or long-term reduction in a person’s capacity to function. A physical or mental disability is a type of morbidity.

An important thing to remember about designating a physical or mental health condition as a disability: what might be a disability for one person might not be considered a disability for another person.

While the definitions of morbidity and disability may seem similar if not the same, they are two distinct concepts. While morbidity refers to psychological or physical illness, or not being healthy in some way. Living with a disability refers to living with a physical or mental impairment. Therefore, it is possible to live with a disability and be perfectly healthy (have no morbidities) (Chamie M., 1995).
Again, our goal is to measure the burden of disease, illness and death using internationally agreed upon and standardized indicators so that comparisons within and between countries can be made. We are interested in identifying the leading causes of illness, disability and death and the distribution/variation of illness, disability and death between and among different populations. Therefore we need a single indicator to compare how distant countries are from a state of good health. The indicator must account for:
- Mortality, morbidity and disability;
- Age, gender and region
- Allow for comparisons across regions and other groupings (Income)
This indicator measures what is referred to as the burden of disease.
Two of the most often used indicators for measuring disease burden are:
- Health Adjusted Life Expectancy (HALE)
- Disability Adjusted Life Expectancy (DALY)
What is a HALE?
HALE is often referred to as healthy life expectancy. Unlike life expectancy, HALE takes into account morbidity. A HALE summarizes the expected number of years a person can expect to live in good health. To calculate a HALE, the years of ill health are weighted according to severity and subtracted from overall life expectancy.
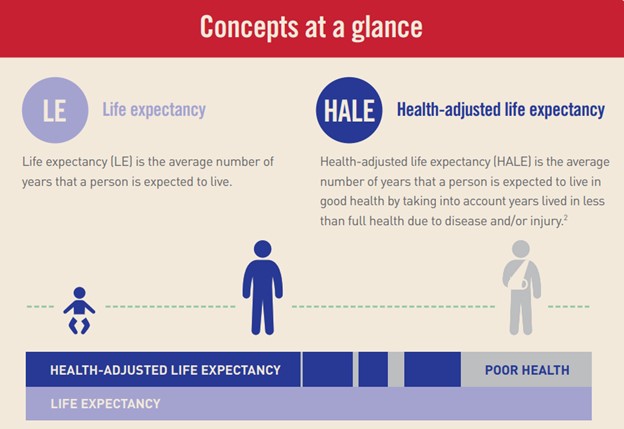
Rights: Copyright © 2021 Provincial Health Services Authority.
Here is a sample calculation:
- Man aged 75 in a given context has a life expectancy of 86
- Estimated years of ill health [in a given population] is 8.5 years
- 86 yrs – 8.5 yrs = 77.5 years is his Health Adjusted Life Expectancy (HALE)

What is a DALY?
DALY is an abbreviation for disability-adjusted life year. It is a universal metric that allows researchers and policymakers to compare very different populations and health conditions across time. A disability-adjusted life year (DALY) equals the sum of years of life lost (YLLs) due to premature death AND years lived with disability (YLDs) similar to the HALE measure.

Here is a sample calculation:
- Person dies at age 70 after having Alzheimer’s disease for 6 years
- Life expectancy at age 70 is 85 years
- Years of Life Lost (YLL) due to premature death = 85 – 70 = 15 years
- Disability weight for Alzheimer’s Disease = 0.5
- Years Lived with Disability (YLD) = 0.5 x 6 = 3 years
- Disability Adjusted Life Years (DALYs) + YLL + YLD = 15 + 3 = 18 years
DALYs are expressed as a rate: Number of DALYs / # in population. DALYs allow us to estimate the total number of years lost due to specific causes and risk factors at the country, regional, and global levels. A country or region that has more DALYs per person (premature death, illness and disability) is one that has a higher burden of disease.
More information can be found at this link which provides many definitions of global health terms: http://www.healthdata.org/gbd/faq
Which indicator, death or DALY provides a better picture of the true health status of a population? ANSWER: DALY because it accounts for both death AND morbidity and disability. Using mortality only would overestimate the health of a population because it does not account for the levels of morbidity and disability in a population. However, both the leading causes of death and DALYs are often used to understand and rank the distribution of diseases, injuries and conditions in global health.

Below we can compare between the Leading Causes of Death and DALY for high income versus low income countries

Section 1.3.4 Risk Factors
As we continue our exploration of the burden of disease, we know the goal is to identify the leading causes of death, illness and disability. You will recall in Section 1.2 that descriptive epidemiology concerns itself with Person, Place and Time. In global health, we often collect and analyze person data according to various social and demographic characteristics such as:
- Age
- Sex
- Education
- Income
- Race/Ethnicity
These characteristics are often used to make comparisons among different population groups. These data are compiled from countries and trends are constructed to understand patterns of disease within groups (males compared to females) or subgroups (males in rural vs urban areas compared to females) over time. These characteristics are sometimes referred to as risk factors. Risk factors can be thought of as attributes, characteristics or exposures that increase the likelihood of a person developing a disease or health disorder. Risk factors can be used to examine the global burden of disease by making comparisons by groups and subgroups with the risk factors. There are other types of risk factors including genetic, environmental exposure, life style and personal behaviors. Those at higher risk could be identified and activities to minimize or prevent risk can be initiated.
Quick Review:
What is a Risk Factor?
To better measure global health, researchers generate systematic estimates of risk factors such as poor diet, tobacco use, and high blood pressure. The research informs policymakers and researchers on the prevalence of risk factors in a population. With this information, targeted interventions can be created to address a population’s most pressing health issues.

Section 1.3.5 Demographic and Epidemiologic Transitions
This section describes two of the most critical concepts that are key to understanding global health. We turn our attention to indepth explorations of population changes and disease changes and the progress we have made over time in improving health globally. Specifically, we will explore:
- The Demographic Transition (Population Shifts)
- The Epidemiologic Transition (Disease Shifts)
Taken together, these are 2 of the most important and foundational concepts in all of global health.
The Demographic Transition
First, let’s look at population changes to understand the impact on people’s health. How do human populations change over time? This can be studied through the field of demography or the study of the changing structure of human populations. In the study of global health, we want to understand how the burden of disease changes as the population changes and what are the implications of these changes on how we should address global health.
Here we must focus on:
- Population Growth
- Population Aging
- Urbanization
- Demographic Divide
Population Growth Trends
We know from demography studies that a majority of population growth will take place in low and middle income countries. Its is estimated that the global population will reach 9.9 billion people by 2050. By the way, how many people are there in the world at the present time? You can click on this to find out the current total population: https://www.worldometers.info/world-population/. High income countries are experiencing low fertility rates such that they are below replacement rates.
Watch this video on Population Growth
Population Aging Trends
We know that we have more people over the age of 65 compared to the number of people aged 15 to 64. This results in a negative Elderly support ratio. The aging population and the shift to a negative elderly support ratio has significant implications for the burden of disease (more non-communicable diseases), health expenditures (increased costs for medical expenses associated with chronic disease maintenance) and how health care will be financed (less younger wage earners to contribute to social security and Medicare the health insurance supports for older adults).
Population Urbanization Trends
The majority of the global population shifted from residing in predominantly rural areas to primarily urban areas in 2005. This demographic shift to urbanization puts pressure on the urban infrastructure including on water and sanitation systems, schools and health services that must increase capacity to provide health care services. Gaps in these infrastructures can have substantial negative consequences for health.
The Demographic Divide
Here we see high income countries experiencing low fertility, decreasing population numbers and aging populations. Similarly, low income countries are experiencing high fertility with steadily increasing population numbers and younger populations.
Let’s look at the trends and impact of these 4 demographic changes and how they all comes together in a change measure over time known as the Demographic Transition in the video below:
Here is a pictorial representation of the Demographic Transition. Note how the shapes of the population pyramids change over time.

Simply put the Demographic Transition represents a shift form high fertility and high mortality to low fertility and low mortality. What causes the Demographic transition to occur?
- Mortality declines with better hygiene and nutrition
- Population grows during the period where mortality declines but fertility remains high (resulting in increased percentage of young people in the population)
- Fertility declines
- Population growth slows and the older share of the population increases as births and deaths equalize
Understanding demographic trends is helpful to addressing key global health issues such as how changes in infrastructure, nutrition, health service access impact on disease trends.
The Epidemiologic Transition
The Epidemiologic Transition looks at disease changes over time to understand the impact on peoples health. Here we must focus on the changes in incidence and prevalence of the following disease categories:
- Communicable (or Infectious) diseases
- Non-communicable (or chronic) diseases
- Injuries (un-intentional)
Lets look at the trends and impact on these 3 disease categories and how they all come together in a change measure over time known as the Epidemiologic Transition through the video below:
Simply put the Epidemiologic Transition is a shift from the burden of disease dominated by communicable diseases to a burden of disease dominated by non-communicable diseases. What causes the epidemiologic transition to occur?
- High and fluctuating mortality rates related to very poor health conditions, epidemics cause by communicable diseases and famine
- Progressive declines in mortality as epidemics become less frequent
- Further declines in mortality, increases in life expectancy, and the predominance of non-communicable diseases
In the series of figures below, the blue block of diseases represent Non Communicable Diseases, the orange block of diseases represent Communicable Diseases and the green block represents injuries. You can set the measures to Deaths or DALYs. What you will see is that the blue block represents an increasing proportion of non communicable diseases while the orange block decreases in proportion representing infectious diseases and the green block representing injuries increases slightly.
GBD World Bank Low Income Countries

GBD World Bank Lower Middle Income Countries

GBD World Bank Upper Middle Income Countries

GBD World Bank High Income Countries

We encourage you to spend some time with a great global health visualization tool. The tool is developed by The Institute for Health Metrics and Evaluation (IHME) an independent global health research center at the University of Washington. Here is a link to the live visualization tool https://vizhub.healthdata.org/gbd-compare/ .
An Exercise: The idea is to watch what happens as you move the year (starting in 1990) forward to 2017. The premise is that all countries are progressing on the health-development link such that as a country develops economically, its disease patterns shift from communicable disease to non-communicable diseases representing the Epidemiologic Transition. This tool allows us to see the Epidemiologic transition taking place over time.
It is interesting to note that this tool has not yet been able to incorporate the impact of COVID on the Epidemiologic transition but assuming the vaccine is rolled to globally in a timely manner, it is likely that COVID 19 will not significantly result in a shift away from the predominance of non communicable diseases in overall global disease burden.
NOTE: You may be familiar with them as they are one of the leading research groups who are monitoring the COVID 19 projections. Here is a link to the COVID 19 area of this group’s website: https://covid19.healthdata.org/united-states-of-america
Section 1.3.6 Levels of Prevention
With our focus on diseases, injuries and conditions, it is time to consider how we might prevent these health conditions and lessen the burden of disease. This can be accomplished through interventions designed to prevent these health concerns in the first place. In global public health, preventive interventions are generally of three (3) types.
- Primary Prevention
- Secondary Prevention
- Tertiary Prevention
Lets explore each one in more detail.
Primary prevention involves intervening before health effects occur. This is often accomplished through strategies such as vaccination, behavior change or banning substances or products. If we think about primary prevention in the context of the current Covid 19 pandemic, primary prevention measures include vaccination, wearing masks, washing hands, personal protective equipment for health workers and travel bans.
Secondary prevention involves screening to identify disease in its earliest stages. Types of screenings include blood tests, blood pressure screenings, mammography and annual physicals. If we think about secondary prevention in the context of the current Covid 19 pandemic, secondary prevention measures include screening individuals coming from Covid 19 ‘hotspots’ and testing of animals and meat.
Tertiary prevention involves managing disease post diagnosis to slow or stop disease progression. This could involve chemotherapy, rehabilitation, screening for complications and isolation of cases. If we think about tertiary prevention in the context of the current Covid 19 pandemic, tertiary prevention measures include provision of antiviral medicine called remdesivir, treatment of symptoms such as shortness of breath, ongoing monitoring for complications and quarantining of persons confirmed to have Covid 19.

Section 1.3.7 Millennium Development (MDGs) and Sustainability Development Goals (SDGs)
The MDGs? The SDGs? What? Let’s explore!
The MDGs
In 2000 the United Nations convened a summit which resulted in the Millennium Declaration. A total of 8 health achievement goals were formulated and participating countries signed a pledge to meet the goals by 2015. The goals are listed in the graphic below.

Rights: All rights reserved United Nations. Good candidate for fair use (educational, non-commercial use)
Well its 2021 now so what happened with the MDGs? There were some successes, but still a long way to go.

The SDGs
In 2012 work began on the ‘Post 2015 framework for international development’ during the UN Conference on Sustainable Development in Rio de Janeiro. This was the beginning of a process to design new global health goals:
“action-oriented, concise and easy to communicate, limited in number, aspirational, global in nature and universally applicable to all countries while taking into account different national realities, capacities and levels of development and respecting national policies and priorities”
The SDGs were adopted in 2015 and there are 17 goals. These are to be achieved over a 15 year period ending in 2030.
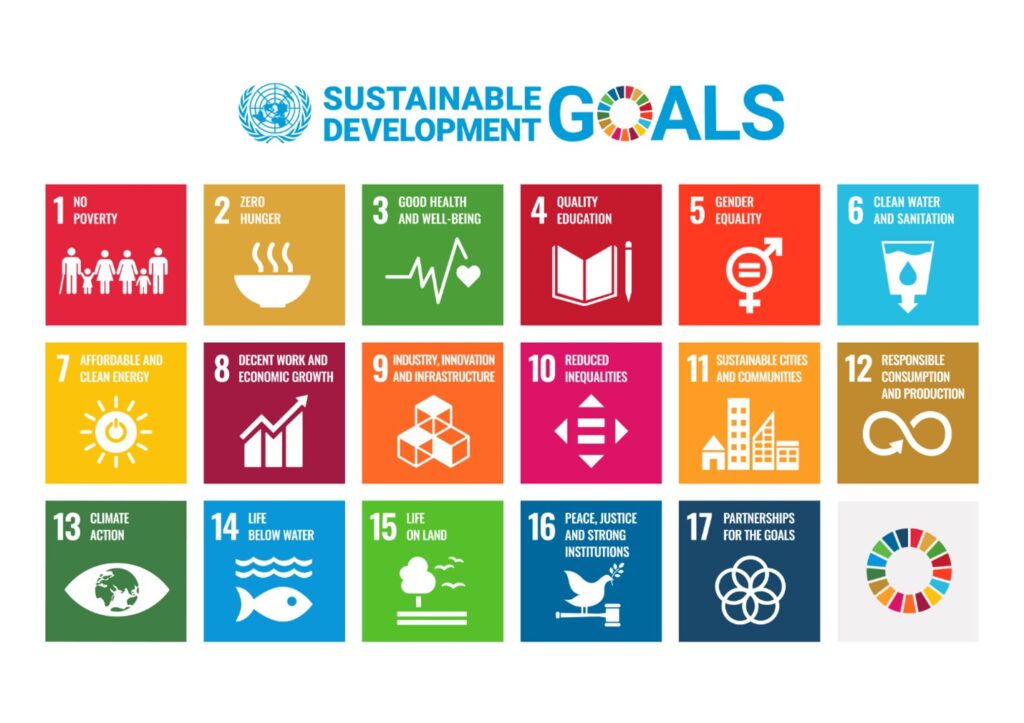
Rights: Informational uses are those that are primarily illustrative, non-commercial, and not intended to raise funds. The SDG Logo: Version 2, the SDG colour wheel and the 17 SDG icons may be used for such informational purposes, and their use does not require prior permission from the United Nations nor the conclusion of a licensing agreement.
The SDGs are designed to recognize the following trends in global health:
- Strong links among health, human development, labor productivity, and economic development
- Health status determined by variety of factors
- Enormous progress in improving health status over last 50 years
- Much progress is the result of public hygiene, better water and sanitation, and better education
- Enormous disparities in health status and access to health services within and across countries
The SDGs are controversial in that some groups feel there are too many and they are too broad. On the other hand, they are more inclusive of the broader social determinants of health and of the environment and consumption. These aspects of the determinants of health will be explored in Sections 1.4 and 1.5 of this textbook.
References:
Chamie M. (1995). What does morbidity have to do with disability?. Disability and rehabilitation, 17(7), 323–337. https://doi.org/10.3109/09638289509166718
OECD (2021), Gross national income (indicator). doi: 10.1787/8a36773a-en (Accessed on 30 August 2021)
Institute for Health Metrics and Evaluation. GBD Compare: Viz Hub. https://vizhub.healthdata.org/gbd-compare/