Key Concepts
- Disease
- Infirmity
- Illness
- Condition
- Communicable/infectious diseases
- Non-communicable diseases
- Injuries
- Mental health
- Morbidity
- Mortality
- Incidence
- Prevalence
- Vital registration
- Life expectancy
- Maternal mortality ratio
- Neonatal mortality rate
- Infant mortality
- Under 5 mortality
Prelim Engagement
For a quick and interesting intro to the material we will cover in this section, take a few minutes to watch and read the following.
1. Watch this video by Hans Rosling:
2. Read this short article.
Section 1.2.1 Disease and Related Concepts
Absence of Disease and Infirmity
You may recall that in Section 1.1 we learned that the World Health Organization (WHO) defined health as ‘ a state of complete physical, mental and social well-being and not merely the absence of disease and infirmity’ (World Health Organization, 1948). Obviously, the presence or absence of disease or infirmity has an impact on health and should be considered as one of the determinants of health. It is interesting to note that the words disease and infirmity are included in this definition of health and that these should be absent for one to be considered to be in a complete state of health or well-being. In the Western biomedical perspective the term disease is defined as ‘a condition of the living animal or plant body or of one of its parts that impairs normal functioning and is typically manifested by distinguishing signs and symptoms’. The word disease comes from a hyphenation of the prefix dis– (lack of) and ease (freedom from pain) in the 14th century. Dis-ease meant lack of ease or not feeling well according to the Oxford English Dictionary. In the 16th century the term disease referred to specific illnesses or sickness (Merriam-Webster, 2021).
Likewise, the word infirmity refers to ‘the quality or state of being of poor or deteriorated vitality.’ It also appears for the first time in the 14th century (Merriam-Webster, 2021). The more common term for infirmity in modern times is condition and we will use that terminology throughout this textbook. It should be noted that from these definitions, disease has a more narrow and identifiable focus through signs, symptoms and pathology that can be observed whereas infirmity or condition suggests a broader focus with less distinguishable or obvious characteristics. This difference will become more clear and important as we continue our journey in defining and measuring the burden of disease.
The Biomedical Paradigm in Global Health and Disease – A Perspective
It is important to acknowledge that Western biomedical understandings of disease and infirmity are generally utilized and dominate much of contemporary global health work. This is due in large part to the influence of the WHO in the post World War II era in which “…the focus was on improving the health of people within individual nations by strengthening their biomedical prevention and treatment capacities” (Singer and Erickson, 2013, p. 16). However, it is critical to change the predominant views of disease and infirmity as narrow medical technical issues because we know there is a human dimension to health that includes cultural beliefs and behaviors. We can continue to learn from other non-Western perspectives in order to ‘see beyond dominant assumptions to assess the actual role of local conditions and social experiences in the making of health and sickness…disease understanding develop at the local level, as do social responses to limit adverse health outcomes through social and cultural adjustments’ (Singer and Erickson, 2013, p. 17) . Such a perspectives include considering the beliefs, voices and cultural practices of marginalized communities (Bautista-Valarezo, Duque, Verdugo Sánchez, 2020). For example, from an indigenous perspective, illness is understood to occur when there is an imbalance among the 4 fundamental dimensions of the spiritual, the intellectual, the physical and the emotional (Committee on Indigenous Health, 1999). This perspective allows for more wholistic, community driven strategies for health promotion and equity.
Disease (and Condition) Causation
Now that we have explored the word disease, let’s examine what causes disease. One of the simplest models of disease causation is the epidemiologic triad or triangle. This model is often used for understanding infectious disease. The triad consists of an external agent, a susceptible host, and an environment that brings the host and agent together. In this model, disease results from the interaction between the agent and the susceptible host in an environment that supports transmission of the agent from a source to that host. Two ways of depicting this model are shown in Figure 2.1.
Agent, host, and environmental factors interrelate in a variety of complex ways to produce disease. Different diseases require different balances and interactions of these three components. Development of appropriate, practical, and effective public health measures to control or prevent disease usually requires assessment of all three components and their interactions.
Figure 1.2.1 Epidemiologic Triad Model
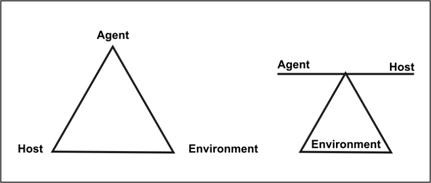
Agent originally referred to an infectious microorganism or pathogen: a virus, bacterium, parasite, or other microbe. Generally, the agent must be present for disease to occur; however, presence of that agent alone is not always sufficient to cause disease. A variety of factors influence whether exposure to an organism will result in disease, including the organism’s pathogenicity (ability to cause disease) and dose.
Over time, the concept of agent has been broadened to include chemical and physical causes of disease or injury. These include chemical contaminants (such as the L-tryptophan contaminant responsible for eosinophilia-myalgia syndrome), as well as physical forces (such as repetitive mechanical forces associated with carpal tunnel syndrome).
Host refers to the human who can get the disease. A variety of factors intrinsic to the host, sometimes called risk factors, can influence an individual’s exposure, susceptibility, or response to a causative agent. Opportunities for exposure are often influenced by behaviors such as sexual practices, hygiene, and other personal choices as well as by age and sex. Susceptibility and response to an agent are influenced by factors such as genetic composition, nutritional and immunologic status, anatomic structure, presence of disease or medications, and psychological makeup.
Environment refers to extrinsic factors that affect the agent and the opportunity for exposure. Environmental factors include physical factors such as geology and climate, biologic factors such as insects that transmit the agent, and socioeconomic factors such as crowding, sanitation, and the availability of health services.
While the Epidemiologic Triad model is most often applied to understanding disease causation, it can also be utilized to understand the causes of conditions/infirmities as in order for a condition to arise there must be a host, an agent (not necessarily a micro-organism) and the environment in which the host and agent interact. In the next section we take an indepth look the major diseases and conditions of concern in global health.
Section 1.2.2 Review of Common Diseases and Conditions
Here we provide a quick review of the top 20 common diseases and conditions worldwide as of 2019 that are of major concern in the field of global health. Many may be familiar to you but others may require a quick review.
Table 1.2.1: Top 20 Global Health Diseases 2019
| 1. Ischaemic heart disease | The most common form of heart disease, in which narrowed or blocked coronary arteries have difficulty supplying sections of the heart muscle with the blood they need (ischemia). |
| 2. Stroke | Blockage or rupture of a blood vessel supplying the brain; often leads to impaired brain function or death. |
| 3. Chronic obstructive pulmonary disease | (COPD) is the name for a group of lung conditions that cause breathing difficulties. It includes emphysema which is damage to the air sacs in the lungs and chronic bronchitis which is long-term inflammation of the airways. |
| 4. Lower respiratory infections | A lower respiratory tract infection (RTI) occurs when there is an infection of the lungs, specifically in the lower airways. This infection is usually caused by a virus, but it can also be caused by bacteria or other less common organisms and pneumonia is an example. |
| 5. Neonatal conditions | Neonatal conditions are defined as conditions occurring during the first month after birth (0- 28 days). Among many neonatal conditions are premature birth, neonatal infections and birth asphyxia which is a lack of oxygen and blood flow to the brain. |
| 6. Trachea, bronchus, lung cancers | Cancer is a disease in which cells in the body grow out of control. When cancer starts in the trachea, it is called trachea cancer. When it starts in the mucous glands and ducts of the lung airways (bronchi) it is called bronchial cancer and when it starts in the lungs, it is called lung cancer. |
| 7. Alzheimer’s disease and other dementias | Alzheimer’s disease is a brain disorder that slowly destroys memory and thinking skills and, eventually, the ability to carry out the simplest tasks. Dementia is the loss of cognitive functioning — thinking, remembering, and reasoning — to such an extent that it interferes with a person’s daily life and activities. |
| 8. Diarrhoeal diseases | Diarrhoeal diseases are usually assoiated with infections in the intestinal tract, which can be caused by a variety of bacterial, viral and parasitic organisms. Infection is spread through contaminated food or drinking-water which results in cholera or from person-to-person as a result of poor hygiene causing rotavirus |
| 9. Diabetes mellitus | A disease in which the body does not properly produce or use insulin, resulting in abnormally high levels of sugar (glucose) in the blood. |
| 10. Kidney diseases | Chronic kidney diseases (CKD) can affect your body’s ability to clean your blood, filter extra water out of your blood, and help control your blood pressure. Main cause of death is lack of dialysis or kidney transplant treatments |
| 11. Cirrhosis of the liver | A chronic disease of the liver that progressively destroys the liver’s ability to aid in digestion and detoxification. |
| 12. Road injury | Road injuries or death due to traffic crashes that result from speeding, impaired/distracted driving, unsafe road quality, non use of vehicle restraints or helmets,, unsafe vehicles or lack of enforcement of traffic laws |
| 13. Tuberculosis | Tuberculosis (TB) is caused by bacteria (Mycobacterium tuberculosis) that most often affect the lungs and spread from person to person through the air |
| 14. Hypertensive heart disease | A group of heart diseases caused by high blood pressure. Hypertension is a major risk factor for stroke, especially hemorrhagic and lacunar strokes, because it puts excess stress on the walls of blood vessels and damages their delicate inner lining. |
| 15. Colon and rectum cancers | Colon cancer is a type of cancer that begins in the large intestine (colon). Rectal cancer is a type of cancer that begins in the rectum. In both cases it usually begins as small, noncancerous (benign) clumps of cells called polyps that form on the inside of the colon or rectum. |
| 16. Stomach cancer | Stomach cancer, also called gastric cancer, begins when cells in the stomach start to grow out of control. |
| 17. Self-harm | deliberate nonsuicidal injury to one’s own body tissue, as cutting or burning the skin, or pulling out hair, in a physical manifestation of emotional distress |
| 18. Falls | advertently coming to rest on the ground, floor or other lower level, excluding intentional change in position to rest in furniture, wall or other objects |
| 19. HIV/AIDS | Abbreviation for human immunodeficiency virus, the virus that leads to acquired immunodeficiency syndrome (AIDS). HIV damages immune cells so that they are no longer able to fight off other infections. |
| 20. Breast cancer | Breast cancer is a disease in which cells in the breast grow out of control. There are different kinds of breast cancer. The kind of breast cancer depends on which cells in the breast turn into cancer. |
A good medical terminology glossary resource can be found at: Medical Glossary – D – Medical Dictionary online-medical-dictionary.org
Section 1.2.3 Classification of Diseases and Conditions
The Trio of Disease Classification
Given that this is a global health course we will be talking about different diseases throughout the course – not too much of a surprise, right? 🙂
In public and global health we do, however, have a certain way of talking about groups of diseases and how diseases are classified. This will be especially important when we turn to conversations about the Global Burden of Disease. In global health there are in fact many ways to classify and talk about diseases – you will hear terms like ‘neglected tropical diseases’, ‘emerging infectious diseases’, ‘re-emerging infectious diseases’, ‘diseases of poverty’, ‘diseases of wealth’ and others. We will discuss all of these in more detail later in the textbook.
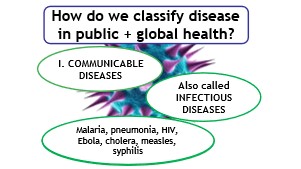
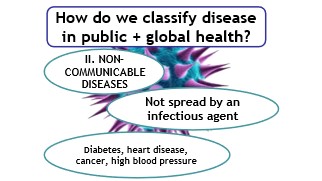
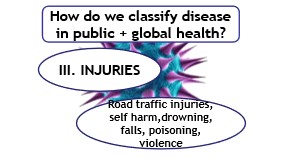
The most common way the field of global health classifies and talks about diseases is by putting diseases into three groups as follows:
- Group I (1): Communicable Diseases
- Group II (2): Non-communicable Diseases
- Group III (3): Injuries
Please note that the Roman numeral convention is used to label the 3 major groups of disease categories.
Group I: Communicable Diseases are also referred to as infectious diseases. As we noted above, the disease agent is a micro-organism which results in an infection of the host in their environment. From Table 2.1 above, we see several examples of communicable diseases in the top 20 list such as Lower Respiratory Infections (pneumonia), Diarrhoeal Diseases (Cholera), Tuberculosis and HIV/AIDS. Notice there are four (4) diseases listed in the Group I: Communicable Diseases category in Table 2.1.
If you are interested in how communicable disease are defined, this is a great resource: Case Definitions for Infectious Conditions Under Public Health Surveillance (cdc.gov)
Group II: Non-Communicable Diseases (NCDs) are also referred to as chronic diseases. In this case, the host is exposed to a number of non-infectious agents such physical or behavioral factors (i.e., exercise, diet) in their environment. From Table 2.1 above, we see multiple examples of NCDs in the top 20 list such as Heart Diseases, Stroke, COPD, Cancers, Diarrheal Diseases, Kidney Diseases, Cirrhosis, Diabetes and Alzheimer’s Disease and other Dementias. Notice there are twelve (12) diseases listed in the Group II: Communicable Diseases category in Table 2.1.
Group III: Injuries. Injuries do not fit neatly into the classic notion of disease. However, they are an important contributor to how we conceptualize and measure the burden of disease because they can result in the development of a disease (accidental exposure to chemicals resulting in skin or respiratory diseases). Similar to NCDs, the host is exposed to non-infectious agents in their environment (often the workplace). From Table 2.1 above, we see multiple examples of Injuries in the top 20 list such as Road Injuries, Falls and Self Harm. Notice there are three (3) injury groups listed in the Group III: Injuries category in Table 2.1.
If you take a careful look at Table 2.1, you will notice that one of the diseases listed in the Top 20 is missing, namely Neonatal Conditions. This grouping of conditions includes a variety of diseases that are infectious such as sepsis (a blood infection), chronic such as Down Syndrome (a birth defect) and result from injuries at birth such as birth asphyxia (a birth complication).
A Comment on Mental Health/Neurological Diseases and Conditions
It is important to note that while mental health/neurological diseases and conditions are often grouped as non-communicable or chronic diseases, they are sometimes listed as a fourth group that includes three (s) subcategories: 1) Mental health disorders such as Depression and Bipolar Disorder; neurological diseases such as Alzheimer’s and Parkinson’s disease and substance use disorders such as alcohol or opioid use (GHE, 2020).
In Table 2.2 below you will see a summary of Disease Classifications and some examples.
Table 1.2.2 Global Health Disease Classifications and Some Examples
| Disease Type | Disease Group Number | Examples |
| Communicable or Infectious Disease | I | Lower Respiratory Infections (pneumonia) Diarrhoeal diseases (cholera) Tuberculosis HIV/AIDS Ebola Measles Syphillis |
| Non-Communicable Diseases (NCDs) or Chronic Diseases | II | Heart Disease Stroke COPD Cancers Diabetes Alzheimer’s Disease and Related Dementias Chronic Kidney Disease Cirrhosis of the liver Hypertensive Heart Disease |
| Injuries | III | Road Injuries Self Harm Falls |
Section 1.2.4 Introduction to Epidemiology
Context: Section 2.4 is made up of excerpts from a self study training manual for learning the fundamentals of Epidemiology and Biostatistics. The entire course is available online from the Centers for Disease Control and Prevention at Principles of Epidemiology: Home|Self-Study Course SS1978|CDC
Definition
Now that we have an understanding of how diseases and conditions are classified, we will explore how we identify diseases and conditions in these categories and why these classifications are important. Public health provides us with an excellent approach for learning about diseases and conditions known as Epidemiology. You were introduced to the term epidemiology in Section 1.1 but now we are going to go more in depth. The word epidemiology comes from the Greek words epi, meaning on or upon, demos, meaning people, and logos, meaning the study of. Epidemiology is the study of the distribution and determinants of health conditions or events among populations and the application of that study to control health problems. The words in bold are highlighted for the following reasons.
Study – Epidemiology is a scientific discipline with sound methods of scientific inquiry at its foundation
Distribution – is concerned with the frequency and pattern of health events in a population
Frequency refers to the number of health events such as the number of cases of Covid 19 or diabetes in a population
Pattern refers to the occurrence of health-related events by time, place, and person. Time patterns may be annual, seasonal, weekly, daily, hourly, weekday versus weekend, or any other breakdown of time that may influence disease or injury occurrence. Place patterns include geographic variation, urban/rural differences, and location of work sites or schools. Personal characteristics include demographic factors which may be related to risk of illness, injury, or disability such as age, sex, marital status, and socioeconomic status, as well as behaviors and environmental exposures.
Determinants are the causes and other factors that influence the occurrence of disease and other health-related events. They assess whether groups with different rates of disease differ in their demographic characteristics, genetic or immunologic make-up, behaviors, environmental exposures, or other so-called potential risk factors. Ideally, the findings provide sufficient evidence to direct prompt and effective public health control and prevention measures.
Health-related states or events
The term health-related states or events may be seen as anything that affects the well-being of a population. This can refer to diseases, injuries, birth defects, maternal-child health, occupational health, and environmental health. They can also include behaviors related to health and well-being, such as amount of exercise and seat belt use and even genetics.
Specified populations
The epidemiologist is concerned about the collective health of the people in a community or population. In other words, the epidemiologist’s “patient” is the community. Therefore, the clinician and the epidemiologist have different responsibilities when faced with a person with illness. For example, when a patient with diarrheal disease presents, both are interested in establishing the correct diagnosis. However, while the clinician usually focuses on treating and caring for the individual, the epidemiologist focuses on identifying the exposure or source that caused the illness; the number of other persons who may have been similarly exposed; the potential for further spread in the community; and interventions to prevent additional cases or recurrences. This idea should be familiar to you from Section 1.1 in which public health and clinical medicine were discussed.
Application
Epidemiology is not just “the study of” health in a population; it also involves applying the knowledge gained by the studies to community-based practice. The practice of epidemiology is both a science and an art. The epidemiologist uses the scientific methods of descriptive and analytic epidemiology as well as experience, epidemiologic judgment, and understanding of local conditions in “diagnosing” the health of a community and proposing appropriate, practical, and acceptable public health interventions to control and prevent disease in the community.
Summary
Epidemiology is the study (scientific, systematic, data-driven) of the distribution (frequency, pattern) and determinants (causes, risk factors) of health-related states and events (not just diseases) in specified populations (patient is community, individuals viewed collectively), and the application of (since epidemiology is a discipline within public health) this study to the control of health problems.
Uses and Functions of Epidemiology
Epidemiology and the information generated by epidemiologic investigation have been used in many ways. Two common uses are described below.
- Assessing the Community’s Health
Public health officials responsible for policy development, implementation, and evaluation use epidemiologic information as a factual framework for decision making. To assess the health of a population or community, relevant sources of data must be identified and analyzed by person, place, and time (descriptive epidemiology).
- What are the actual and potential health problems in the community?
- Where are they occurring?
- Which populations are at increased risk?
- Which problems have declined over time?
- Which ones are increasing or have the potential to increase?
- How do these patterns relate to the level and distribution of public health services available?
Hippocrates, the father of medicine, was also a public health oriented person and maybe even an early epidemiologist. Notice how in his famous piece ‘On Airs, Waters and Places’ he recognizes that time (seasons), place (particular locality, wind and waters) and person (life style behaviors) are important to investigating disease.
On Airs, Waters, and Places
By Hippocrates
Translated by Francis Adams
PART 1
Whoever wishes to investigate medicine properly, should proceed thus:
in the first place to consider the seasons of the year, and what effects
each of them produces for they are not at all alike, but differ much
from themselves in regard to their changes. Then the winds, the hot
and the cold, especially such as are common to all countries, and
then such as are peculiar to each locality. We must also consider
the qualities of the waters, for as they differ from one another in
taste and weight, so also do they differ much in their qualities.
In the same manner, when one comes into a city to which he is a stranger,
he ought to consider its situation, how it lies as to the winds and
the rising of the sun; for its influence is not the same whether it
lies to the north or the south, to the rising or to the setting sun.
These things one ought to consider most attentively, and concerning
the waters which the inhabitants use, whether they be marshy and soft,
or hard, and running from elevated and rocky situations, and then
if saltish and unfit for cooking; and the ground, whether it be naked
and deficient in water, or wooded and well watered, and whether it
lies in a hollow, confined situation, or is elevated and cold; and
the mode in which the inhabitants live, and what are their pursuits,
whether they are fond of drinking and eating to excess, and given
to indolence, or are fond of exercise and labor, and not given to
excess in eating and drinking.
2. Searching for Causes
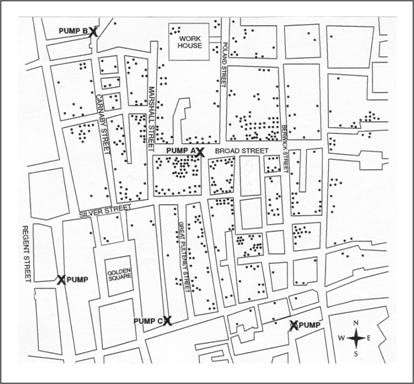
Much epidemiologic research is devoted to searching for causal factors that influence one’s risk of disease. Ideally, the goal is to identify a cause so that appropriate public health action might be taken. Epidemiology often provides enough information to support effective action. One well known example involves the removal of the handle from the Broad St. pump following John Snow’s investigation of cholera in the Golden Square area of London in 1854. In the diagram Snow mapped cases of cholera occurring in the local area. The X’s indicate the locations of the hand pump. As you can see, most of the cases occurred around the pump on broad street. Snow had the pump handle removed and the cases of cholera decreased significantly. He reasoned that the water coming from the pump was the cause of the excess in cholera cases.
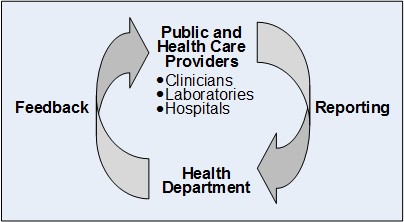
Public Health Surveillance
Public health surveillance is the ongoing, systematic collection, analysis, interpretation, and dissemination of health data to help guide public health decision making and action. Surveillance is equivalent to monitoring the pulse of the community. The purpose of public health surveillance, which is sometimes called “information for action,” is to understand the ongoing patterns of disease occurrence and disease potential so that investigation, control, and prevention measures can be applied efficiently and effectively. This is accomplished through the systematic collection and evaluation of relevant health information and the dissemination of these data and their interpretation to those involved in disease control and public health decision making.
Types of Epidemiology
The field of epidemiology can be divided into 2 branches often referred to as Descriptive epidemiology and Analytical epidemiology. Descriptive epidemiology aims to organize and summarize data regarding the persons affected (e.g., the characteristics of those who became ill), time (e.g., when they become ill), and place (e.g., where they might have been exposed to the cause of illness). Analytic epidemiology seeks to understand what health problem occurs and why. Analytic epidemiology uses comparison groups to provide baseline or expected values so that associations between exposures and outcomes can be quantified and hypotheses about the cause of the problem can be tested. We will focus on analytic epidemiology methods in Section 1.3. In short, epidemiologists often ask the 5 W’s (Who, When, Where, What, Why).
In section 1.2, we will focus our attention on understanding diseases and conditions from a descriptive epidemiology perspective. Descriptive epidemiology covers person, time and place.
As with all scientific endeavors, the practice of epidemiology relies on a systematic approach. In very simple terms, the epidemiologist:
- Counts cases or health events, and describes them in terms of time, place, and person;
- Divides the number of cases by an appropriate denominator to calculate rates; and
- Compares these rates over time or for different groups of people.
Before counting cases, however, the epidemiologist must decide what a case is. This is done by developing a case definition.
Defining a case
A case definition is a set of standard criteria for classifying whether a person has a particular disease, syndrome, or other health condition. Some case definitions, particularly those used for global health surveillance, have been developed and adopted as international standards that ensure comparability. Use of an agreed-upon standard case definition ensures that every case is equivalent, regardless of when or where it occurred, or who identified it. Furthermore, the number of cases or rate of disease identified in one time or place can be compared with the number or rate from another time or place. For example, with a standard case definition, global public health officials can compare the number of cases of COVID 19 that occurred in Senegal in March of 2000 with the number that occurred there in March of 1999. Or they could compare the rate of COVID 19 Senegal in 2000 with the global rate in that same year. When everyone uses the same standard case definition and a difference is observed, the difference is likely to be real rather than the result of variation in how cases are classified.
Epidemiologists strive for similar comprehensiveness in characterizing an epidemiologic event, whether it be a pandemic of influenza or a local increase in all-terrain vehicle crashes. However, epidemiologists tend to use synonyms for the five W’s listed above: case definition (What), person (Who), time (When), place (Where) and causes/risk factors/modes of transmission (Why).
Compiling and analyzing data by who, time and place is desirable for several reasons.
- First, by looking at the data carefully, the epidemiologist becomes very familiar with the data. He or she can see what the data can or cannot reveal based on the variables available, its limitations (for example, the number of records with missing information for each important variable), and its eccentricities (for example, all cases range in age from 2 months to 6 years, plus one 17-year-old.).
- Second, the epidemiologist learns the extent and pattern of the public health problem being investigated — which months, which neighborhoods, and which groups of people have the most and least cases.
- Third, the epidemiologist creates a detailed description of the health of a population that can be easily communicated with tables, graphs, and maps.
- Fourth, the epidemiologist can identify areas or groups within the population that have high rates of disease.
This information in turn provides important clues to the causes of the disease, and these clues can be turned into testable hypotheses. Let’s take a more in depth look at Person, Time and Place characteristics.
Person
“Person” attributes include age, sex, ethnicity/race, and socioeconomic status.
Because personal characteristics may affect illness, organization and analysis of data by “person” may use inherent characteristics of people (for example, age, sex, race), biologic characteristics (immune status), acquired characteristics (marital status), activities (occupation, leisure activities, use of medications/tobacco/drugs), or the conditions under which they live (socioeconomic status, access to medical care). Age and sex are included in almost all data sets and are the two most commonly analyzed “person” characteristics. However, depending on the disease and the data available, analyses of other person variables are usually necessary. Usually epidemiologists begin the analysis of person data by looking at each variable separately. Sometimes, two variables such as age and sex can be examined simultaneously. Person data are usually displayed in tables or graphs.
Age. Age is probably the single most important “person” attribute, because almost every health-related event varies with age. A number of factors that also vary with age include: susceptibility, opportunity for exposure, latency or incubation period of the disease, and physiologic response (which affects, among other things, disease development).
Sex. Males have higher rates of illness and death than do females for many diseases. For some diseases, this sex-related difference is because of genetic, hormonal, anatomic, or other inherent differences between the sexes. These inherent differences affect susceptibility or physiologic responses.
Ethnic and racial groups. Sometimes epidemiologists are interested in analyzing person data by biologic, cultural or social groupings such as race, nationality, religion, or social groups such as tribes and other geographically or socially isolated groups. Differences in racial, ethnic, or other group variables may reflect differences in susceptibility or exposure, or differences in other factors that influence the risk of disease, such as socioeconomic status and access to health care.
Socioeconomic status. Socioeconomic status is difficult to quantify. It is made up of many variables such as occupation, family income, educational achievement or census track, living conditions, and social standing. The variables that are easiest to measure may not accurately reflect the overall concept. Nevertheless, epidemiologists commonly use occupation, family income, and educational achievement, while recognizing that these variables do not measure socioeconomic status precisely.
Time
The occurrence of disease changes over time. Some of these changes occur regularly, while others are unpredictable. Two diseases that occur during the same season each year include influenza (winter) and West Nile virus infection (August–September). In contrast, diseases such as hepatitis B and salmonellosis can occur at any time. For diseases that occur seasonally, health officials can anticipate their occurrence and implement control and prevention measures, such as an influenza vaccination campaign or mosquito spraying. For diseases that occur sporadically, investigators can conduct studies to identify the causes and modes of spread, and then develop appropriately targeted actions to control or prevent further occurrence of the disease.
In either situation, displaying the patterns of disease occurrence by time is critical for monitoring disease occurrence in the community and for assessing whether the public health interventions made a difference.
Secular (long-term) trends. Graphing the annual cases or rate of a disease over a period of years shows long-term or secular trends in the occurrence of the disease. Health officials use these graphs to assess the prevailing direction of disease occurrence (increasing, decreasing, or essentially flat), help them evaluate programs or make policy decisions, infer what caused an increase or decrease in the occurrence of a disease (particularly if the graph indicates when related events took place), and use past trends as a predictor of future incidence of disease.
Seasonality. Disease occurrence can be graphed by week or month over the course of a year or more to show its seasonal pattern, if any. Some diseases such as influenza are known to have characteristic seasonal distributions. Seasonal patterns may suggest hypotheses about how the infection is transmitted, what behavioral factors increase risk, and other possible contributors to the disease or condition.
Place
Describing the occurrence of disease by place provides insight into the geographic extent of the problem and its geographic variation. Characterization by place refers not only to place of residence but to any geographic location relevant to disease occurrence. Such locations include place of diagnosis or report, birthplace, site of employment, school district, hospital unit, or recent travel destinations. The unit may be as large as a continent or country or as small as a street address, hospital wing, or operating room. Sometimes place refers not to a specific location at all but to a place category such as urban or rural, domestic or foreign, and institutional or noninstitutional.
Analyzing data by place can identify communities at increased risk of disease. Even if the data cannot reveal why these people have an increased risk, it can help generate hypotheses to test with additional studies. For example, is a community at increased risk because of characteristics of the people in the community such as genetic susceptibility, lack of immunity, risky behaviors, or exposure to local toxins or contaminated food? Can the increased risk, particularly of a communicable disease, be attributed to characteristics of the causative agent such as a particularly virulent strain, hospitable breeding sites, or availability of the vector that transmits the organism to humans? Or can the increased risk be attributed to the environment that brings the agent and the host together, such as crowding in urban areas that increases the risk of disease transmission from person to person?
Section 1.2.5 From Cases to Rates and Measures of Risk
Now that we understand the concept of a case and that a case can be described by person, time and place, we turn to the concept of a rate. Keep in mind that a case can be in the form of a disease, an injury or a condition.
Definition of Rate
In epidemiology, a rate is a measure of the number/frequency of cases (of a disease, injury, condition) that occurs in a defined population over a specified period of time. Because rates put disease frequency in the perspective of the size of the population, rates are particularly useful for comparing the frequency of diseases, injuries or conditions in different locations, at different times, or among different groups of persons with potentially different sized populations.
To a non-epidemiologist, rate means how fast something is happening or going. The speedometer of a car indicates the car’s speed or rate of travel in miles or kilometers per hour. This rate is always reported per some unit of time. Epidemiologists use the term rate to refer to a proportion or fraction with case counts in the numerator and the size of the population in the denominator during some period of time (such as a year). There are many rates used in global health and we will now explore some of the most common.
Key Health Indicators
If you remember back to the discussion in Section 1.1, we said that public health as a field is, generally, focused on measuring health challenges and identifying solutions to those challenges on a population level rather than the individual level.
In the field of global health we often use Key Health Indicators expressed as rates in order to determine the health status of a population and compare health status between two or more populations.
When we refer to a populations we can mean a group of individuals on a number of different levels — a population could refer to a population of a village, a city, a region, a country or an international region like ‘Southeast Asia’, ‘North America’ or ‘Sub-Saharan Africa.’
In order to identify health disparities – “differences in health that are closely linked with social or economic disadvantage” – we often use Key Health Indicators to see if we can observe differences in rates of diseases, injuries and conditions and how they impact on health outcomes such as death or illness.
There are a number of health indicators used in global health but the ones described below are among the most basic key indicators used to measure population health.
Mortality Rate
A mortality rate is a measure of the frequency of occurrence of death in a defined population during a specified interval. The formula for the mortality of a defined population, over a specified period of time, is:
Deaths occurring during a given time period ∕ Size of the population among which the deaths occurred × 10n
In global health, values of 1,000 and 100,000 are both used for 10n for most types of mortality rates.
Table 1.2.3 summarizes the formulas of frequently used mortality measures. A variety of mortality rates describe deaths among specific groups, particularly by age or sex or by cause.
Key Mortality Indicators
Table 1.2.3 Frequently Used Measures of Mortality
| Measure | Numerator | Denominator | 10n |
| Crude death rate | Total number of deaths during a given time interval | Size of population during the same time interval | 1,000 or 100,000 |
| Cause-specific death rate | Number of deaths assigned to a specific cause during a given time interval | Size of population during the same time interval | 100,000 |
| Under-5 mortality (child mortality rate) | Probability that a newborn baby will die before reaching the age of 5 | Number of live births during the same time interval (per 1,000 live births) | 100 |
| Neonatal mortality rate | Number of deaths among children < 28 days of age in a given year | Number of live births during the same time interval (per 1,000 live births in that year) | 1,000 |
| Infant mortality rate | Number of deaths among children < 1 year of age during a given time interval | Number of live births during the same time interval (per 1,000 live births in that year) | 1,000 |
| Maternal mortality ratio | Number of women who die as a result of pregnancy and childbirth complications | Number of live births during the same time interval (per 100,000 live births in that year) | 100,000 |
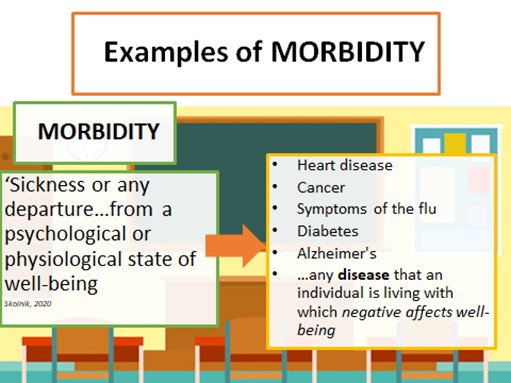
Morbidity Rate
Morbidity has been defined as any departure, subjective or objective, from a state of physiological or psychological well-being. In practice, morbidity encompasses disease, injury, and condition and refers to the number of persons who are ill.
Now, try to distinguish morbidity statistics from mortality statistics. I’ve used an example from COVID-19 globally as of January 18 2021.
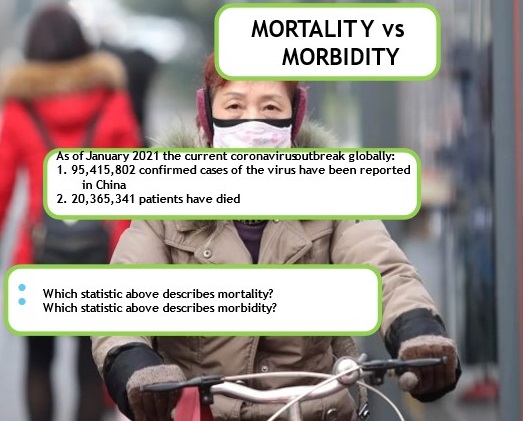
Source: Statistics 1 & 2: https://coronavirus.jhu.edu/map.html
So, what did you think?
If you said that Statistic 1 was an example of morbidity then you are correct!
Cases indicates morbidity – “sickness or any departure from…psychological or physiological well-being” (Skolnik, 2020) – related to COVID-19.
Statistic 2, referencing the number of deaths globally, is a mortality statistic.
If you are interested in accurate statistics on the state, national and global levels here are two of the most reliable data sets:
State of Illinois: Illinois Department of Public Health COVID-19 statistics
National and global: Johns Hopkins University Coronavirus Resource Center
Morbidity and mortality measures are often the same mathematically; it’s just a matter of what you choose to measure, illness or death. Mortality and morbidity statistics are frequently cited in public and global health to track the number of deaths from a disease or the spread and magnitude of disease outbreaks.
Morbidity Measures
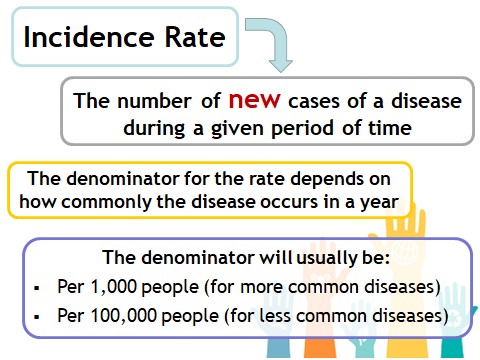
The two primary measures of morbidity are prevalence and incidence.
- Prevalence reflects the presence of disease in a population.
- Incidence rates reflect the occurrence of new disease in a population.

We will reference the terms prevalence and incidence often when discussing different diseases, injuries and conditions, especially current/emerging global health emergencies such as the COVID-19 disease.
Prevalence
A measure of morbidity frequency characterized by the number of persons in a population who are ill at a given time (prevalence). For example, 70 influenza case-patients in March 2021 reported in Colombia.
Incidence
Another measure of morbidity frequency characterized by the number of persons who become ill (incidence). For example, 70 new cases of breast cancer per 1,000 women per year. As you see below, the denominator of rates in global health depend on how common the disease is — more common diseases will be measured out of 1,000 people while less common diseases will be measured out of 100,000 people. The time period for a rate is often one year.
Take a look at this hypothetical example to illustrate some of the key vocabulary we just discussed.
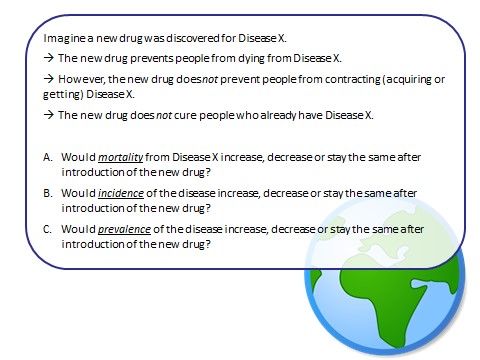
So, what do you think?
A. Because the new drug prevents people from dying, mortality from Disease X will decrease.
B. Because the new drug does not prevent people from contracting (getting) Disease X incidence – or the number of new cases of the disease – will probably continue to increase.
This does depend a bit on the transmission rate – how quickly the disease is spread and if anyone is already immune to the disease – but assuming that the disease transmits relatively easily then we can say incidence will probably continue to increase.
C. Because the new drug also does not cure anyone who already has the disease then we can assume that prevalence – or the number of people who have the disease – will also increase; often as incidence increases so does prevalence.
Section 1.2.6 Level of Disease
Level of disease
The amount of a particular disease that is usually present in a community is referred to as the baseline or endemic level of the disease. This level is not necessarily the desired level, which may in fact be zero, but rather is the observed level. In the absence of intervention and assuming that the level is not high enough to deplete the pool of susceptible persons, the disease may continue to occur at this level indefinitely. Thus, the baseline level is often regarded as the expected level of the disease.
While some diseases are so rare in a given population that a single case warrants an epidemiologic investigation (e.g., rabies, plague, polio), other diseases occur more commonly so that only deviations from the norm warrant investigation. Sporadic refers to a disease that occurs infrequently and irregularly. Endemic refers to the constant presence and/or usual prevalence of a disease or infectious agent in a population within a geographic area. Hyperendemic refers to persistent, high levels of disease occurrence.
Occasionally, the amount of disease in a community rises above the expected level. Epidemic refers to an increase, often sudden, in the number of cases of a disease above what is normally expected in that population in that area. Outbreak carries the same definition of epidemic, but is often used for a more limited geographic area. Cluster refers to an aggregation of cases grouped in place and time that are suspected to be greater than the number expected, even though the expected number may not be known. Pandemic refers to an epidemic that has spread over several countries or continents, usually affecting a large number of people.
Epidemics occur when an agent and susceptible hosts are present in adequate numbers, and the agent can be effectively conveyed from a source to the susceptible hosts. More specifically, an epidemic may result from:
- A recent increase in amount or virulence of the agent,
- The recent introduction of the agent into a setting where it has not been before,
- An enhanced mode of transmission so that more susceptible persons are exposed,
- A change in the susceptibility of the host response to the agent, and/or
- Factors that increase host exposure or involve introduction through new portals of entry.(47)
The previous description of epidemics presumes only infectious agents, but non-infectious diseases such as diabetes and obesity exist in epidemic proportion in the world today.(51, 52)
Section 1.2.7 Vital Registration
As you perhaps already can tell, we use data and statistics – or the analysis of data – a lot in public and global health. Data and statistics guide most of the important decisions made in this field, including:
- Prioritizing health challenges
- Creating and evaluating solutions to address health challenges
- Dividing up resources between countries and populations to address health challenges
In the ongoing pandemic, countries around the world have been relying on data and statistics available on the daily, weekly and monthly spread, infection rate and hospitalization rates of COVID-19 to plan their shelter in place policies and the phased ‘re-opening’ of different parts of countries.
Of course, there are many other practical factors that need to be considered as well in global health decision making, as the COVID-19 situation showed us – the stoppage of work, international trade and travel around the world is having detrimental effects on individuals’ lives as they cannot work.
→ Follow this link to a fantastic photojournalist project in the Democratic Republic of the Congo documenting the effects of COVID-19 and the challenges of responding to COVID.
So, while data and statistics have guided many decisions around the world in the past months, the practicalities of our global, national and local systems also dictate how and when public and global health decisions are ultimately made and implemented. However, even considering the practical side of public and global health practice, without sound data it is impossible to make public and global health decisions which will actually address the health challenges facing different populations around the world.
To create an effective solution, you have to first know and understand the problem, right?
One way that we gather this kind of data on the health status of populations around the world is through vital statistics. Vital statistics are generally collected through vital registration systems, sometimes also called civil registration systems. These systems generally record:
- Births
- Deaths
- Causes of death
Watch this video clip to understand more about the challenges many low and middle income countries face in implementing and maintaining these systems.
As we will also see throughout the course, there are certain populations which are particularly vulnerable to health challenges and lack of access to resources – and these populations often include women, particularly mothers, and children.
Watch this video clip to understand how well-functioning Vital Registration systems can help to improve the lives of mothers and newborns
Conclusion
Just as we opened this section acknowledging the varied understandings of disease and infirmity from both Western biomedical and Indigenous perspective, we conclude with some thoughts on the use of population health rates and statistics in global health work. It is well recognized that dominant statistical definitions, measurements and methodologies are designed to reflect and reinforce the characteristics of the modern nation state. Indigenous scholars argue that population statistics ‘tend to constitute Indigenous peoples as deficient and that these portrayals can, and do, restrict and inhibit other ways of understanding or using statistical data by, and for, Indigenous peoples’ (Walter and Andersen, 2013. p. 16). In order to address this situation, global health professionals should work toward epidemiologic methods that ‘operates within, and reflects, Indigenous historical, cultural, and racial values, priorities and frameworks’ (Walter and Andersen, 2013, p.16). It is essential to break the cycle of traditional approaches to data collection and interpretation of statistics in global health.
Supplementary Resources:
Communicable (infectious) diseases “are caused by microorganisms such as bacteria, viruses, parasites and fungi that can be spread, directly or indirectly, from one person to another. Some are transmitted through bites from insects while others are caused by ingesting contaminated food or water,” (WHO, n.d.)
Non-communicable (chronic) diseases are not passed from person to person and “tend to be of long duration and are a result of a combination of genetic, physiological, environmental, and behavioral factors,” (WHO, 2021).
Injuries are “the physical damage that results when a human body is suddenly subjected to energy in amounts that exceed the threshold of physiological tolerance, or from a lack of one or more vital elements,” (WHO, 2007)
Mental illness is “a state of well-being in which an individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and is able to make a contribution to his or her community. Multiple social, psychological, and biological factors determine the level of mental health of a person at any point of time. For example, violence and persistent socio-economic pressures are recognized risks to mental health,” (WHO, 2018).
Morbidity refers to having a disease or symptom of a disease or refers to the amount of disease within a population (National Cancer Institute, n.d.)
Mortality rate is the measure of frequency of death in a specific population during a specific interval (CDC, 2012)
- Health metrics / Key health status indicators
- https://data.worldbank.org/indicator
- WB indicator glossary with visuals for each
- WHO Core Health Indicators
- www.datatopics.worldbank.org/sdgatlas
References:
Bautista-Valarezo, E., Duque, V., Verdugo Sánchez, A.E. et al. Towards an indigenous definition of health: an explorative study to understand the indigenous Ecuadorian people’s health and illness concepts. Int J Equity Health 19, 101 (2020). https://doi.org/10.1186/s12939-020-1142-8
Centers for Disease Control and Prevention. (2012). Section 3: Mortality Frequency Measures. https://www.cdc.gov/csels/dsepd/ss1978/lesson3/section3.html
Committee on Indigenous Health. The Geneva Declaration on the Health and Survival of Indigenous Peoples 1999. WHO, Geneva. (WHO/HSD/00.1.).
Global Health Estimates 2019: Deaths by Cause, Age, Sex, by Country and by Region, 2000-2019. Geneva, World Health Organization; 2020.
National Cancer Institute. (n.d.). Morbidity. National Institutes of Health. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/morbidity
Merriam-Webster. (n.d.). Disease. In Merriam-Webster.com dictionary. Retrieved August 30, 2021, from https://www.merriam-webster.com/dictionary/disease
Merriam-Webster. (n.d.). Infirmity. In Merriam-Webster.com dictionary. Retrieved August 30, 2021, from https://www.merriam-webster.com/dictionary/infirmity
Scully J. L. (2004). What is a disease?. EMBO reports, 5(7), 650–653. https://doi.org/10.1038/sj.embor.7400195
Singer, M., & Erickson, P. I. (2013). Global health: An anthropological perspective. Waveland Press.
Snow J. Snow on cholera. London: Humphrey Milford: Oxford University Press; 1936.
Walter, M., & Andersen, C. (2016). Indigenous statistics: A quantitative research methodology. Routledge.
World Health Organization. (n.d). Communicable diseases. WHO Regional Office for Africa. https://www.afro.who.int/health-topics/communicable-diseases
World Health Organization. (2021). Noncommunicable diseases. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
World Health Organization. (2018). Mental health: strengthening our response. https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response
World Health Organization (2007). The role of public health in injury prevention. WHO European Regional Office. https://www.euro.who.int/__data/assets/pdf_file/0010/98803/Policy_briefing_1.pdf
WHS 2020 Visual Summary